Post-Menopausal Bleeding – A Cause For Cancer?
Posted By Dr. Deepti Asthana on 05-11-2021
Menopause happens when a woman has gone a year without having her menstrual cycle. This event is caused by an average fall in hormones that a woman would often encounter in her 40s or 50s.
When a woman enters menopause, she usually does not anticipate having any additional bleeding. Women may, however, have extra vaginal bleeding on occasion. If she has gone through menopause, physicians consider the bleeding abnormal, and she should see her doctor.
Causes
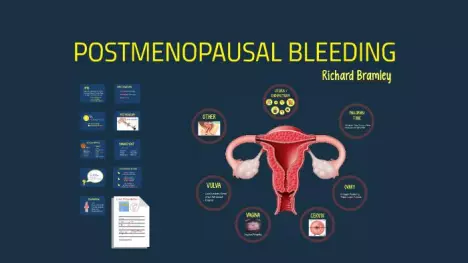
There are many reasons for postmenopausal haemorrhage. Some of the most prevalent causes are as follows:
Endometrial atrophy: When the hormone oestrogen ceases to be generated due to menopause, a woman's endometrial lining may thin. As a consequence, the endometrial lining may be more prone to bleeding.
Endometrial hyperplasia: This disorder causes the uterine lining to thicken rather than thin, resulting in excessive or irregular bleeding. The most prevalent cause of this illness is an overabundance of oestrogen without the hormone progesterone to balance it out. Endometrial hyperplasia may occasionally progress to endometrial cancer.
Endometrial cancer: Endometrial carcinoma is a kind of cancer that affects the lining of the uterus. Endometrial cancer is thought to be responsible for 10% of uterine bleeding in postmenopausal women.
Polyps: Polyps are growths that may form on the uterine lining. They are generally benign, however, they might produce unusual or excessive bleeding. Polyps may develop within the cervical canal on occasion. When this happens, a woman may suffer bleeding while having intercourse.
Clotting issues are another possibility, although less likely, cause of postmenopausal bleeding.
Endometritis: Endometritis is an infection of the uterine lining that causes pelvic trauma and bleeding from the urinary system. Hormone therapy may result in postmenopausal bleeding as a side effect. Many women may suffer breakthrough bleeding within the first six months of beginning hormone replacement treatment.
When a woman has vaginal bleeding, she should see her doctor regardless of the underlying reason.
Diagnosis:
A doctor will begin an examination for postmenopausal bleeding by questioning the patient about her symptoms. A doctor will most likely inquire about when she first noticed her signs, how much she bleeds, and if she has a family history of postmenopausal bleeding.
A doctor may prescribe one or more of a variety of tests based on a woman's symptoms. Among the tests performed to determine the source of postmenopausal bleeding are:Endometrial biopsy: This process includes introducing a short, thin tube into the vagina to reach the cervix and collect a sample of uterine tissue lining. This tissue may then be analysed to see whether it contains any aberrant cells, such as malignant cells.
Hysteroscopy: This technique includes a doctor putting an instrument with a narrow, illuminated camera on end into the uterus to inspect the interior and lining. The method may assist a doctor in identifying polyps or abnormal growths.
Transvaginal ultrasound: This method includes putting a special ultrasound probe into the vagina for a doctor to see the uterus from the bottom of the uterus rather than the lower abdomen. While most of these tests may be done at a doctor's office, some, such as a D&C, are usually done in a hospital or surgical centre.
Treatment
Treatments for postmenopausal bleeding are often dependent on the underlying cause of the bleeding.
A doctor may use the information acquired from the tests to choose the best course of therapy. Here are some instances of therapies for specific underlying causes:
Polyps: Polyp treatment may include surgical excision of the polyps so that they no longer bleed.
Endometrial cancer: Endometrial cancer is often treated by removing the uterus and any adjacent lymph nodes to which the disease may have spread. A hysterectomy is a medical term for this treatment. Depending on the extent of cancer spread, a woman may additionally need chemotherapy and radiation treatments.
Endometrial hyperplasia: Women with this disease may be prescribed progestins, which assist to keep the endometrial lining from getting excessively thick. However, a doctor may advise frequent screening for malignant cells within the uterus to verify that they do not have endometrial cancer.
A doctor may give vaginal oestrogen if a woman has vaginal bleeding owing to endometrial thinning. This drug may help to minimise the consequences of tissue thinning.
Call and book your appointment for abnormal bleeding with Dr. Deepti Asthana, gynaecologist in gurugram.
In case you are looking for the best gynaecologist in Gurugram, you should meet Dr Deepti Asthana. She is a senior gynaecologist in Fortis hospital, gurugram and director of KALOSA Clinics. She is well educated, highly experienced, and an excellent mentor and supporter to her patients. She makes sure she explains the disease aetiology to all her patients and treats the patients in the most efficient way possible. She is an excellent surgeon, and in case of surgery is required for any of your ailments, you can blindly rely on her. So next time you are stuck on where to go, kindly contact her in Fortis hospital or Kalosa Clinic.